 Alta Vista Healthcare & Wellness Centre, LLC (Alta Vista), a skilled nursing facility in Riverside, California, and its management company, Rockport Healthcare Services (Rockport), have agreed to pay the federal government to settle false claims kickback scheme, officials announced Wednesday.
Alta Vista Healthcare & Wellness Centre, LLC (Alta Vista), a skilled nursing facility in Riverside, California, and its management company, Rockport Healthcare Services (Rockport), have agreed to pay the federal government to settle false claims kickback scheme, officials announced Wednesday.
They will pay a total of $3.825 million to resolve allegations that they paid kickbacks to doctors to make patient referrals.
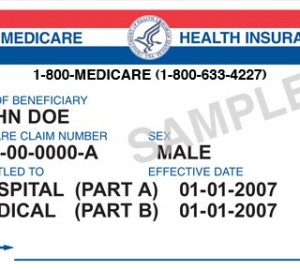
The Anti‑Kickback Statute prohibits offering or paying remuneration to induce the referral of items or services covered by Medicare, Medicaid, and other federally funded programs.
 It is intended to ensure that improper financial incentives do not compromise medical decision-making and are instead based on the patient’s best interests.
It is intended to ensure that improper financial incentives do not compromise medical decision-making and are instead based on the patient’s best interests.
From 2009 through 2019, Alta Vista, under the direction and control of Rockport, gave certain physicians extravagant gifts, including expensive dinners for the physicians and their spouses, golf trips, limousine rides, massages, e-reader tablets, and gift cards worth up to $1,000.
Separately, Alta Vista paid these physicians monthly stipends of $2,500 to $4,000, purportedly for their services as medical directors.
At least one purpose of these gifts and payments was to induce these physicians to refer patients to Alta Vista.
“Kickbacks can impair the independence of physician decision-making and waste taxpayer dollars,” said Principal Deputy Assistant Attorney General Brian M. Boynton, head of the Justice Department’s Civil Division. “The department is committed to preventing illegal financial relationships that undermine the integrity of our public healthcare programs.”
California Attorney General Rob Bonta said: “When a healthcare company cheats and offers kickbacks to gain an unfair advantage, it jeopardizes the health and wellbeing of those who rely on its services. These illegal schemes also make public services and programs costlier, and ultimately waste valuable taxpayer dollars.”
The defendants’ conduct allegedly resulted in false claims to Medicare and California’s Medicaid programs, the latter of which is jointly funded by the federal government and California.
 Under the settlement, they will pay $3.2 million to the federal government and $596,700 to California.
Under the settlement, they will pay $3.2 million to the federal government and $596,700 to California.
The settlement announced Wednesday stems from a whistleblower complaint filed in 2015 by a former Alta Vista accounting employee, Neyirys Orozco, pursuant to the qui tam provisions of the False Claims Act, which permit private persons to bring a lawsuit on behalf of the government and to share in the proceeds of the suit.
In this case, Orozco will receive $581,094 as her share of the federal government’s recovery.
In addition to resolving their False Claims Act liability, Alta Vista and Rockport have entered into a five-year Corporate Integrity Agreement with the HHS-OIG which requires, among other compliance obligations, an Independent Review Organization’s review of Alta Vista’s and Rockport’s physician relationships.
The federal settlement in this matter illustrates the government’s emphasis on combating healthcare fraud. One of the most powerful tools in this effort is the False Claims Act.
Tips and complaints from all sources about potential fraud, waste, abuse, and mismanagement, can be reported to the HHS-OIG, at 800‑HHS‑TIPS (800-447-8477).
This matter was handled by the Civil Division’s Commercial Litigation Branch, Fraud Section, the U.S. Attorney’s Office for the Central District of California, and the California Department of Justice, with investigative support from the HHS-OIG

