A federal jury in Baltimore convicted a Maryland doctor Monday for submitting over $15 million in false and fraudulent claims to Medicare and insurance companies.
A federal jury in Baltimore convicted a Maryland doctor Monday for submitting over $15 million in false and fraudulent claims to Medicare and insurance companies.
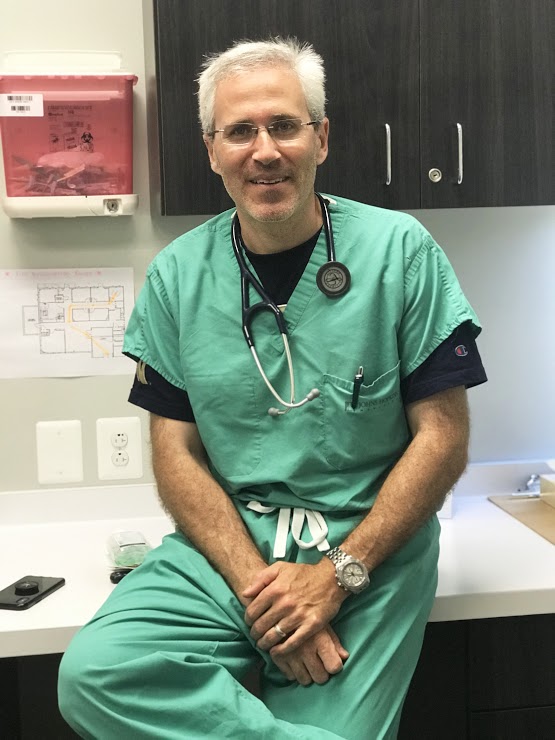
Dr. Ron Elfenbein fraudulently billed Medicare and Insurance companies for patients who received COVID-19 tests at his testing sites.
According to the evidence during trial, Elfenbein, 49, of Arnold, was an owner and the medical director of Drs ERgent Care LLC, dba First Call Medical Center and Chesapeake ERgent Care.
 Drs ERgent Care operated multiple drive-through COVID-19 testing sites in Anne Arundel and Prince George’s counties.
Drs ERgent Care operated multiple drive-through COVID-19 testing sites in Anne Arundel and Prince George’s counties.
Elfenbein instructed the employees of Drs ERgent Care that, in addition to billing for COVID-19 tests, the employees were to bill for high-level evaluation and management visits.
In reality, these visits were not provided to patients as represented.
Rather, Elfenbein instructed his employees that the patients were “there for one reason only – to be tested,” that it was “simple and straightforward,” and that the providers were “not there to solve complex medical issues.”
 Elfenbein ordered these high-level visits to be billed for all patients, including those who were asymptomatic, getting tested for COVID-19 for their employment requirements, and being tested for COVID-19 so that they could travel.
Elfenbein ordered these high-level visits to be billed for all patients, including those who were asymptomatic, getting tested for COVID-19 for their employment requirements, and being tested for COVID-19 so that they could travel.
Through Drs ERgent Care, Elfenbein caused the submission of millions of dollars in claims to Medicare and a commercial insurer for tens of thousands of high-level visits that were not provided as represented and were ineligible for reimbursement.
 The jury convicted Elfenbein of five counts of healthcare fraud.
The jury convicted Elfenbein of five counts of healthcare fraud.
He is scheduled to be sentenced on Nov. 7 and faces a maximum penalty of 10 years in prison on each of the five counts.
Elfenbein is the first doctor convicted at trial by the Justice Department for healthcare fraud in billing for office visits in connection with patients seeking COVID-19 tests.
(Related Maryland Investigative News Report filed last month about Unwanted COVID-19 Testing Kits)
The HHS-OIG, DCIS, FBI, and OPM-OIG investigated the case.
In the past three years, the Health Care Fraud Strike Force has rooted out healthcare fraud related to the COVID-19 pandemic.
To date, 53 defendants have been charged in nationwide COVID-19 Health Care Fraud Enforcement Actions for causing over $784 million in loss associated with the pandemic, including this case.
 Trial Attorney D. Keith Clouser of the Criminal Division’s Fraud Section and Assistant U.S. Attorney Matthew P. Phelps for the District of Maryland are prosecuting the case.
Trial Attorney D. Keith Clouser of the Criminal Division’s Fraud Section and Assistant U.S. Attorney Matthew P. Phelps for the District of Maryland are prosecuting the case.
The Fraud Section leads the Criminal Division’s efforts to combat health care fraud through the Health Care Fraud Strike Force Program.
Since March 2007, this program, comprised of 15 strike forces operating in 25 federal districts, has charged more than 5,000 defendants who collectively have billed the Medicare program for more than $24 billion.
More information can be found at www.justice.gov/criminal-fraud/health-care-fraud-unit.