Genomic Health, Inc. (GHI), a Delaware corporation headquartered in Redwood City, California, agreed to pay $32.5 million to resolve allegations that it violated the False Claims Act.
Genomic Health allegedly did this by engaging in a nationwide scheme to improperly bill Medicare for certain laboratory tests used to diagnose and treat cancer patients. GHI is a wholly owned subsidiary of Exact Sciences Corporation, which acquired GHI in November 2019.
According to federal officials, the claims resolved by the settlement are allegations only, and there has been no determination of liability.
GHI provides genomic-based clinical diagnostic tests. Its principal test, Oncotype DX®, is used for patients diagnosed with breast, colon and prostate cancer.
The federal government alleged that GHI perpetrated a scheme to evade Medicare’s 14-Day Rule, which governs the billing of genomic laboratory tests like Oncotype DX®.
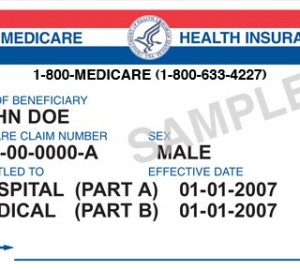
 During some or all of the time period covered by the settlement, Medicare’s 14-Day Rule prohibited laboratories from separately billing Medicare for covered tests if a physician ordered the test within 14 days of the patient’s discharge from a hospital stay in an inpatient or outpatient setting.
During some or all of the time period covered by the settlement, Medicare’s 14-Day Rule prohibited laboratories from separately billing Medicare for covered tests if a physician ordered the test within 14 days of the patient’s discharge from a hospital stay in an inpatient or outpatient setting.
For inpatient beneficiaries, such tests were covered under a lump-sum payment hospitals receive from the Medicare Program called the Diagnosis-Related Group (DRG) payment.
For outpatient beneficiaries, Medicare’s 14-day Rule required (for most of the relevant time) tests ordered within 14 days of the patient’s discharge to be billed to the hospital. Still, the hospital could then seek reimbursement from Medicare.
 However, if the test was performed more than 14 days after discharge from a hospital stay, either in an inpatient or outpatient setting, then Medicare’s 14-Day Rule permitted laboratories to bill Medicare directly for the test.
However, if the test was performed more than 14 days after discharge from a hospital stay, either in an inpatient or outpatient setting, then Medicare’s 14-Day Rule permitted laboratories to bill Medicare directly for the test.
“This settlement rightly requires the payment of double damages caused by delayed tests for cancer patients for no reason other than to circumvent a Medicare requirement and allow improper payment to GHI,” said U.S. Attorney Breon Peace for the Eastern District of New York. “We will continue to enforce Medicare rules to protect the program and its vital role in our health care system, especially for those suffering from the ravages of cancer.”
The civil settlement includes the resolution of allegations brought in two separate actions filed against GHI under the False Claims Act’s qui tam or whistleblower provisions.
Under those provisions, private parties can file an action on behalf of the United States and receive a portion of any recovery.
In this case, the relator’s share from the proceeds of the settlement will be $5.6 million.
The investigation and resolution of this matter illustrates the government’s emphasis on combating healthcare fraud.
One of the most powerful tools in this effort is the False Claims Act. Tips and complaints from all sources about potential fraud, waste, abuse and mismanagement can be reported to HHS at 800-HHS-TIPS (800-447-8477).

